FAQs
BY
DENTISTS
Why? Because I get asked the same questions quite a lot... :)
1) What type of composite do you use?
This varies depending on case. I have used most brands and in many cases use multiple brands depending on what I want to achieve. Mainly I like to use Supreme, Asteria, GC, Renamel & Hri. I have 2 light cures that I use 3M Elipar DeepCure and VALO by Ultradent (I generally cure min 10 seconds and at multiple angles where possible). Most composites nowadays are very good and that it is mainly operator skill and knowledge provides the best results. I generally try to use a little modelling resin by GC or Brush and Sculpt by Cosmedent. I use GC/Cosmedent no 1 brushes and smile line have angled and non angled auto-claveable versions. If I have used a bulk fill it will be stated under the image (normally we will use filtek one or sdr and build no more than 2-4mm increments) or see below question regarding cores. Composites should retain their polish for at least 3-5 years, the following may help: use a brand with good scientific and long term follow up, layer correctly, use a good curing light, deep glycerine cure, ensure methodical polishing protocol and marginal finishing. For composite and porcelain repairs we tend to use Co-Jet by 3M and on occasion porcelain etch and silane from Ultradent. Remember for anterior bonding success make sure you always check the occlusion and anterior guidance, use strict bonding protocols, provide a night guard or retainer and warn the patient of potential fractures, chips and stains in the future. I try to calibrate my cleaning on a regular basis with caries indicator i.e. Bio clear or Ultra dent or Kuraraye.
2) What liner do you use?
I like Theracal, SDR, ML from GC and superlow flow Tokuyama. The situations I use them and why I discuss on my course. I try not drill away 'healthy' stained tooth tissue where possible and either opaque/abrade or for anteriors internally whiten (google search internal tooth bleaching). We like to use around 1-2mm flowable composite as base liner to the margins, round internal line angles, help with seal and create a radio-opaque masking layer.
3) What brand of rubberdam do you use?
My favourite for photographs is nictone blue heavy (email: [email protected] ps. I do not know any other suppliers), non-latex I like unodent and isodam. I do the majority of my work under rubber dam isolation for patient comfort, improved bonding, control and safety (plus lots more reasons - the benefits of working under dam are endless!). Sometimes if I cannot go through the contact initially I will pre open the contacts with an IPR strip or work under split dam. With onlays (in general we use emax) you may need to use a floss tie to keep the dam seated. With class V restorations I generally work under split dam. I pre wedge for at least 5 mins for all class 2s to allow better seating and haemostasis when I place the dam on. Sometimes the dam looks a different colour during the procedure because of either i) amount of light ii) different brand or shade of dam used iii) sometimes we change the dam during the procedure iv) the flash exposure can be different. We keep the dam clean by doing the following: i) working clean is a mindset ii) wipe the dam clean if needed iii) protect the dam with wedges iv) if there is a tear, loss of seal or amalgam residue I sometimes will change the dam. We prefer to floss secure and place clamp first and then secure the rest (but we change our protocols depending on the situation which we will discuss on the course https://www.youtube.com/watch?v=gfxJUojcmSs). The dam is often changed if we are replacing an amalgam to prevent contamination or if the patient needs a restroom break. Also after air abrasion with ethanol we find the colour of the dam is more matt and is duller (sometimes if handpicks have been over oiled this can create issues).
3) What burs do you use?
I have my own kit available from Komet please contact them on [email protected]. The step by step process of what burs and when is discussed on each teaching module. For occlusal reduction we primarily work on the inclines with a small rugby/flame or round diamond followed by polishing. For preps we like to use the ultrasonic Massironi tip kit also.
4) What camera do you use?
I have a Nikon D7200, D850 with nissin/nikon twin flashes for anterior work with AXIS following eLAB protocol (https://www.emulation.me) and Canon R5 with ring flash +/- polarised filter (polar_eyes) for posteriors when needed. Both with 100 mm macro lens and black out contrasters by smile line (flexipalette). I shoot in both RAW and JPEG backed up on a secure network. My microscope (CJ Optik) runs through a full frame Sony A7Rii and record video at 4K (I prefer camera mounts over mobile). Here is a helpful video about set up and settings: www.youtube.com/watch?v=JQDASOGQp-M
Here are helpful articles about set up and settings:
https://www.nature.com/articles/sj.bdj.2009.607
https://iaaesthetics.com/change-these-6-settings-to-dramatically-improve-your-dental-photography/
With regards to loupes I use x7.5 or microscope for everything including exams. Check out Bryant dental, cj optik and Zeiss. I have a bambach and brumaba ergonomic chairs with arm supports.
5) What matrix do you use?
I like bioclear biofit HD curved (transparent available from bio clear website or optident in UK), tor vm 50micron (silver) and palodent v3 rings. Sometimes for deep margin cases I customise a tofflemire or use a garrison deep margin matrix. I rarely use a Bio-Clear anterior matrix (personal preference) and have my own technique (especially for black triangles) that I discuss on the anterior course. Of recent we have been using polydentia double ring system with a stiff molar matrix. For more information please visit: http://www.polydentia.ch. Other rings and systems such as Garrison etc are fine, if you find what you use works for you then I am happy for you - theres no best system. We tend to build our proximal walls with one shot injection moulding around 1mm thick and cured min 40secs at multiple angles. If we need a large wedge in perio cases we tend to use polydentia haem wedges or the large diamond bioclear wedges. If you see long thin normal wood colour wedges then I am using slim jim wizard wedges by Waterpik.
6) What kit do you use for occlusal carving and layering?
I use the LM arte kit from SI. Namely the fissura and a cosmedent paintbrush (you can also get disposable brush tips from Ivoclar and Smile line). Hu-friedy composite instruments are also recommended. We always like to blend the composite to create smooth margins using the paint brush.
7) What do you use for disinfection? What are the bubbles?
Chlorhexidine solution 2% (www.qedendo.co.uk) and the bubbles are a secret!
8) What cavity preparation or abrasion do you use?
I use twin chamber aquacare by Velopex. I prefer 29micro Alumina and then finish with bioactive glass sylc (1-2 bar) to remove aprismatic enamel rods to ensure no white lines and best possible adhesion.
9) What do you use to cut the gum?
Thermacut bur dentsply or laser. If the margin is a bone level I will carry out sectional surgical crown lengthening to the correct biological width.
10) What clamps do you use?
This varies depending on the situation please attend my course for exact explanations. My own custom rubber dam kit is hopefully coming soon for more information please contact us directly via email.
11) Where have you finished your margin?
I always prefer supra gingival so I can see and create a smooth finish line. I prefer to always finish on sound tooth but sometimes prefer deep margin elevation where I feel more comfortable if it is raised for cementation purposes. I do not recommend that you carry out deep margin elevation in either composite or rmgic without being trained by someone experience as it is one of the most technically demanding procedures in restorative dentistry. If in doubt please refer your case to a periodontist for surgical crown lengthening or a more experienced clinician. Case selection is critical in such cases.
www.sodymd.com.ar/pdf/deep-margin-elevation-a-paradigm%20shit.pdf
www.styleitaliano.org/pdf_article.php?id=11320
With direct composites I always try to remove any unsupported enamel and this drives weather I keep an existing contact or not. If in doubt use an ultrasonic scaler to remove any thin or unsupported tissue whatever is remaining is normally good to retain for bonding purposes post air abrasion. Specific protocols are discussed on the hands on courses.
12) What is injection moulding?
This involves heated composite around 55 degrees (for the benefits of heated composite: https://www.researchgate.net/publication/7770241_Monomer_Conversion_of_Pre-heated_Composite) sometimes with the addition of flowable composite and injected into the cavity and cured multiple times at multiple angles. Here is a video: www.youtube.com/watch?v=6qvaXLNsq0o
13) Do you layer posteriors if so why?
I like layering obliquely as you get multiple cures for a 'strong' restoration and can mimic the beauty of nature. Recreating anatomy requires patience and skill and requires one to develop the fun artistic side of their dentistry. Also by recreating cusp inclines that we see in natural teeth promotes a more stable positive occlusion for patients. In general I will use a dark chromatic dentine shade (a4) followed by a lighter enamel shade (a2/a3). We always try to shade match at the beginning before the dehydration/desiccation effect of the rubberdam (hence sometimes immediately after placement you will see a discrepancy in the colour between the composite and the tooth - within a few hours (if layered correctly) you restoration will be almost invisible. Some people say that replicating anatomy increases the risk of fracture of a composite, to this I can categorically say that in over a decade of layering I have never seen one of my composites split where I have placed a fissure. Although it is true that if your fissures are too deep this can attract food and plaque therefore you must be appropriately trained in such techniques.
14) How do you keep the anatomy?
This is an expansive question which I answer on my course but I advise to always takes a photo of your occlusion before you start and remember your anatomical landmarks. Sometimes you will see a picture where I have restored a fractured or worn cusp with composite and you cannot understand how. This may because I have calculated the room I have available and/or it is part of a full mouth rehabilitation or orthodontic case. Remember do not make judgements when you do not have all the information this is a dangerous. Also I may add that just because some people can do something that you cannot do, does not mean they are wrong and vice versa, always speak to fellow clinicians with respect and assume they are innocent unless proven otherwise. The process of replicating anatomy is discussed on the educational course.
15) What cement and core material do you use?
I generally use heated composite for my core material or a dual cure composite (Ivoclar or G-Aenial GC) but also like to cement with it or variolink esthetic for anterior veneers. The general advice is use a cement and bond made by the same company as they have been designed for optimum bond strength. For RBB's we use PANAVIA 2.0. For posteriors I prefer composite/relyx ultimate or estecem II. A good paper on cementation with composite: www.sciencedirect.com/science/article/pii/S0109564117302579#.WiJMaFfaOAY.facebook
16) Do you treat dentists or HCA's?
Yes I treat many dentists and healthcare professionals, please contact [email protected] or visit www.tahadental.co.uk for referrals. Clinic availability is currently in our custom facility in Oxfordshire only. Also if intra oral photographs and radiographs can be forwarded pre operatively it would help thank you.
17) Could I come watch you at work to observe?
Unfortunately due to the nature of our clientele who want their privacy maintained this is not currently possible. In the future we will be running live patient courses at our training facility please visit www.drth.co.uk/courses.
18) Do you do your anterior work freehand or via a putty stent from a diagnostic wax up?
I always try to do a diagnostic wax up and putty matrix in order to plan the case better. The only time I do not is in an emergency situation where I do a quick A3 body composite mock up without full bonding and create a putty matrix from this. For tooth wear cases we generally get a diagnostically mounted articulated study models in CR (after using the KOIS deprogrammer) and give the patient a night guard at the end of treatment such as a michigan splint if apt.
19) What composite fissure and layering tints do you use?
I like to use the tints kit from Cosmedent (anteriors)/Micerium HFO/Ivoclar brown for posteriors or mix brown and black GC essentia. We normally add tints to reflect nature at the end if it is present in the remaining dentition. Staining/tinting is not essential to function, we recommend that you always discuss this and gain consent from your patient beforehand. Some people say that it does create a more bio mimetic restoration and seals the fissure patterns but this is down to the individual. We layer the tints anteriorly before the final enamel layer and posteriorly as the last addition. I am not worried about wash out as I cure with glycerin gel and find that this is not an issue.
20) Why do you like using zirconia?
Because the soft tissue reacts very well to it (especially if I carry out a vertical or cracked tooth preparation). It is stronger than lithium disilicate. In general I will choose monolithic but in aesthetically demanding cases I will choose layered zirconia . Fit surface is sandblasted 29 micron then Scotch bond/Silane applied and then cemented. One can also use Ivoclean (by Ivoclar Vivadent) to clean the fit surface after try if needed. Most of my bonded posterior indirects will be eMax unless otherwise stated.
21) What is a Vertical or BOPT preparation?
Please visit: www.sweden-martina.com/en_gb/product/bopt_technique-17191/products_for_bopt_technique-17190/bopt_technique-17189.html
22) Do you do any online videos?
Please visit my youtube page (search Dr Thomas Dentist) or visit www.dentinaltubules.com
23) What impression materials do you use?
I currently use 3M impregum soft quick, imprint 4 and honigum by DMG. But also have access to digital scanners such Trios/Medit/iTero.
24) What is your polishing protocol for composites?
We use the Komet, EVE and 3M spiral polishers and finishers with Micerium goats hair brush and sometimes use enamelize paste by Cosmedent (for anterior polishing we normally spend around 15-30 minutes). I also have a specific polishing protocols for different scenarios that I discuss on my course. Heres a quick video: https://www.youtube.com/watch?v=FU7TGWyG-h8
25) What bond do you use?
We generally use Optibond fl and Scotch bond universal. I prefer 4th generation total etch protocols but on occasion (where I deem necessary) I also do carry out selective enamel etch with self etch adhesive (scotch bond or clear fill se). Do not over desiccate dentine.
26) Do you restore one contact at a time?
In general yes as it gives more control. You can start doing multiple contacts in quadrant cases but it depends on cavity design and contact widths needed.
27) Why did you do a composite and not go indirect?
Sometimes the picture you see is part of a longer term plan for the patient and you are just seeing a small window if treatment, which will be restored indirectly at a later date.
if the tooth is heavily restored/cracked or has had a root canal we always generally recommend an indirect cuspal coverage restoration. Some patients due to financial or time restrictions choose composite and are made aware of the risks of their decisions. At the end of the day we as dentists can only guide our patients, give them all the options with the benefits and drawbacks of each, so that they can make an informed decision that is right for them. I would always prefer a direct restoration to doing nothing if a case needs treatment. Sometimes in life we need to pick our battles in order to win the war.
28) What type of temporary do you use?
I tend to use pro-temp or luxa-temp with 3M durelon cement for my temporisation. For veneers we do the same but use spot etch and a little flowable composite if needed.
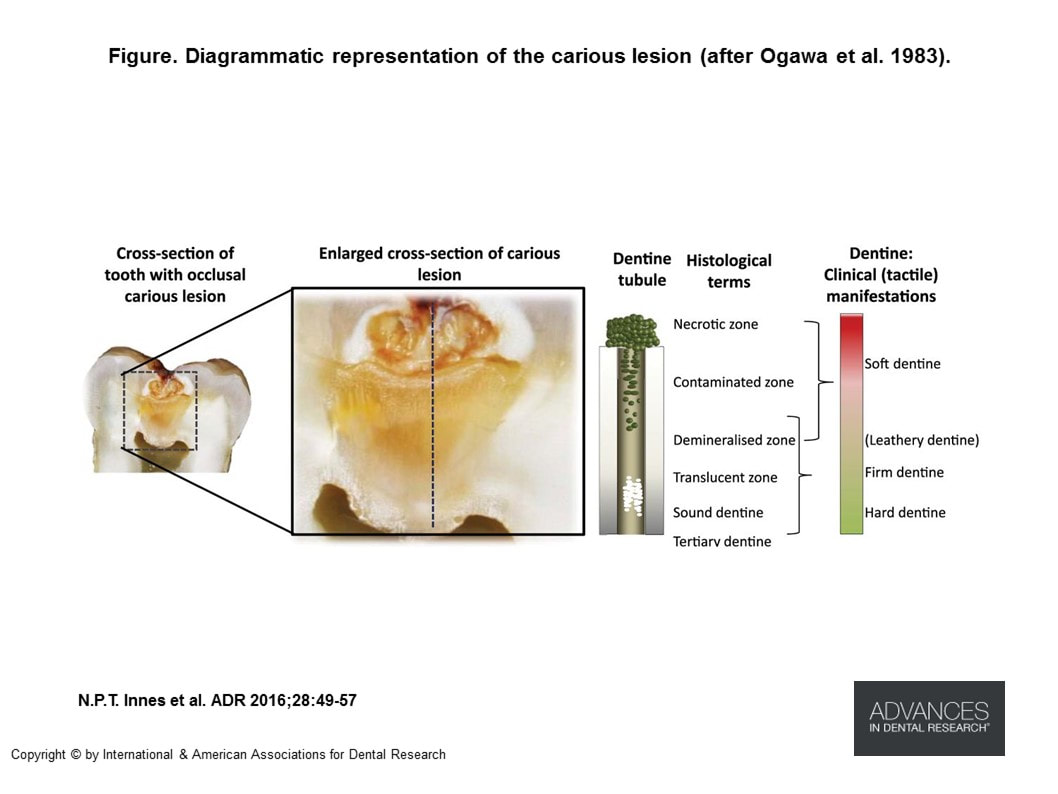
29) Have you left decayed or stained dentine? Why have you done this?
Sometimes there are a number of factors such as decay, cracks, fractures, overhangs, open margins, lack of contact points, patient symptoms, tooth wear, lack of occlusal function or guidance are just some of the reasons treatment is needed. In regards to decay, generally we tend to clean our cavities with slow speed ceraburs by Komet, air abrasion with 29micron Alumina (Aquacare by Velopex) and then disinfection with Chlorhexidine 2% and then selective enamel acid etch follower by optioned fl. We tend to use caries indicator dye (ultra-dent) and remove all softened decay, if the staining is hard and unaffected we tend to leave this and cover with an opaquer (ML from GC). In some instances if decay is very close to the nerve and on discussion with the patient beforehand we 'may' leave this small area alone as long as the margins are clean (1.5-2.0mm circumferential clearance). We may also then place a bio-restorative material over the top to seal in the area such as bio-dentine or MTA or RMGIC, this will then need to monitored and the patient warned of the increased risk of pulpitis requiring root canal therapy in the future.
You can even do a staged approach if worried:
Caries Management: Step-wise Caries Removal
Stepwise excavation is a method of managing deep/extensive/advanced dentinal caries lesions to reduce the risk of pulpal exposures by removing the caries lesion in separate appointments with ≥ 6 month intervals.
Indications:
PTFE is fantastic hydrophobic versatile material. We like to roll it up and use it as cord for retraction purposes (it provides great retraction and is gentle to soft tissues). It is also beautifully malleable to pack against matrices to ensure a tight seal is achieved for injection moulding. We also use it to protect teeth during cementation and bonding phases. There are a million other uses for it that I go through on my course - but suffice to say - I love it!
31) Can you tell me more about this procedure?
Occasionally I will post a case that you may have a lot of questions about.... that’s great, but sometimes I cannot go into too much detail for the following reasons:
I) it is not an appropriate case to discuss on social media. The reason for this is that if I explain a procedure on social media someone may replicate it in their own office without formal education and appropriate research - therefore certain procedures are shown just to encourage you to do further research and study. I will sometimes not post certain radiographs and pictures because I do not feel it is appropriate to discuss such cases in a public arena.
II) Some of the stages will not be explained because I have developed my own protocols that I do not want people to copy without having been appropriately taught and explained on my course.
III) To type the answer will take a long time and will most likely start a time consuming conversation that is best left for a formal course.
iv) If I post an X-ray and you think there is decay or an open margin or anything faulty... I can guarantee you that in 99% of the times it is a burn out/artefact or something that I already know about it. Pointing this out to me provides no information and is not helpful and does not make you appear smarter in anyones eyes. Although if you really think I have made a serious error please do private message me as there is always a chance there is actually a genuine mistake... as nobody is perfect all the time.
v) I am not your short cut to knowledge - do not be lazy and do the work yourself. If in doubt start with google. No one ever gave me any short cuts and I am honestly better for it.
vi) If you are really stuck on a case - please contact your nearest more experienced dentist or specialist for advice.
32) How long did this take you and how much do you charge?
In terms of time for a 2 surface direct restoration we normally book around 45mins-1hr (if it is a deep margin or possible crack case we may book up to around 2 hours depending on the complexity and working under microscope). If we are doing quadrants we generally book 3-4 hours. I have found that in dentistry, time is your friend... the more time you have the more relaxed and better your work will be.
With regards to cost, my advice is that dentistry of the highest standard takes more time therefore you should allow for this and your prices should reflect this. If it is a learning or promotional case and this is explained to the patient then a nominal reduction compared to your normal fee is acceptable. Dentistry requires you to take home a salary for your family so if you are giving a lot of discounts you are undervaluing yourself. Work out your hourly rate to make a modest income and charge this - if your patients value you they will not hesitate to pay you for your time and skill.
33) What articulation do you use?
We use Bausch 100u articulating paper (red and blue) and shimstock. We also use an Artex semi adjustable articulator and facebow (also a KOIS dentofacial analyser where apt). In increasing OVD cases (especially in parafunctional patients), we will deprogram for at least 1 week (Kois deprogrammer) and locate CR as our reference. Then a full mouth diagnostic wax up to the prescribed OVD carried out with a facially driven mock up and facebow. We will then go to prototype phase to assess occlusion, aesthetics and phonetics. Once everyone is happy we will go to final ceramics. To learn more about occlusion I suggest you learn from Kois, Spear or Dawson or someone with equal understanding.
34) Is there enough retention in your prep?
If we have 1.5-2mm ferrule and good circumferential enamel (Lakshmi et al 2006 and Singh S et al 2014 then the retention should be very good if a correct bonding protocol is used (discussed on my course). I sometimes can push the limits of bonding with minimal taper and parametric preparations, I do not recommend that you copy these types of preparations as I have been doing them for over a decade and know when and how they should be done and without expert guidance or instruction they can lead to failure. Also when you see an image of a preparation you do not know the full story of occlusion/symptoms/pt factors so please do not create a judgement based on no information this creates fallacies and inaccurate dogmas. What I can achieve under bonding may not be possible for you or vice versa so I advise all clinicians to work within their safe boundaries unless proper mentoring can be provided.
35) Who is your technician and how do you plan?
Due to working with many different technicians it would be unfair to recommend some and not others. I would advise you to discuss complicated cases with your technician before you start a case. Take photos, articulated study models, facebow, bite registration, shade match and check occlusal stops and try to record CR with a kois Deprogrammer or leaf guage for rehabilitation cases.
36) What courses do you recommend?
Mine! lol But seriously just learn from people that do high level dentistry every day in the real world.
37) How do you make your provisionals?
We normally use protemp or luxatemp (using durelon or relyx temporary cement) and for relining we normally follow this protocol attached is a link to a video: https://www.youtube.com/watch?v=cZQNPDmwdfo
38) Can I discuss one of my cases with you?
Due to medico-legal reasons I cannot discuss individual patient cases. However if you provide articulated study models, photos and radiographs on course days, I will be more that happy to discuss possible treatment options.
39) Your contact point looks light/open?
I never post a finished case with an open contact unless otherwise stated. Sometimes due to angulation of the photo or X-ray it may look like this but in reality it is not. Please remember to not make assumptions on someones work without having all the facts. I am an incredibly experienced clinician and have spent my life teaching and posting cases online so it is rare for someone to pose a question to me that I have never heard before.
40) What is the best way to remove silver fillings?
Rubberdam, good ventilation, high speed suction, masks, eye protetection, amalgam sectioning burs (available from Komet) are all essentials. There are some that believe this should be the protocol: https://iaomt.org/resources/safe-removal-amalgam-fillings/
41) Has a dentist ever drilled one of your natural composites by accident? Or do you replace ‘good’ existing fillings?
Not that I am aware of :) and with regards to replacement generally no if there is nothing wrong with the old restoration then I will avoid replacing it unless requested by the patient or to improve cleaning or function.
42) Are your courses CE verified?
Currently we can only provide verification of attendance and hours attended according to UK GDC guidelines (each registration body across the world is different - please check what the requirements are for your own country). In the future we may apply for this or run the course in North America with a registered partner. Whether you can register the course or not... the education you will receive on the course will help your patients from day 1 and improve your level of dentistry, that is what it is all about at the end of the day.
43) Can I do module 2 if I have not done module 1?
Due to current demand delegates that have previously completed module one will be given priority and advance notice. Part of the reason for this is that in module one as you will receive exclusive instructions, equipment and training that will make module 2 easier (especially regarding matrixing and isolation). If you really feel you are ready to go straight for module 2 and skip module 1 then let us know.
44) Can you come to my country to teach?
Yes if it is most likely a lecture but less so if a hands on is required. Currently I only do my 2 day hands on training in London because I organise everything myself (which is a lot of hard work!). The reason I do not let corporates organise anything for my courses (unlike most others) is that they simply do not care enough and there is no attention to detail... I organise everything i.e. the bookings, the venue, the teaching, the microscope, the equipment etc etc so I find it very difficult to trust other people to carry out what I want to the same level as myself. This is mainly because I have been let down by so many people before... sometimes if you want something done right you have to do it yourself. In general I prefer that people attend my course as its the most comprehensive learning I can provide anywhere in the world. Should you wish for me to provide a lecture in the UK & Ireland my fee starts from £3500.00 plus travel and accommodation. For international lectures my fee starts from £5000.00 per day plus travel and accommodation. Remember I put thousands of hours into original slides from scratch to create a custom lecture for each event. So the fee must take that into consideration plus the loss of earnings from travelling. I NEVER lecture for free unless for a charitable cause that I can accommodate. I currently do not do online seminars or lectures as I prefer face to face teaching.
45) Should I use GIC for Zirconia Crowns?
The most important factor with crowns is the preparation and the remaining substrate. Too many times as dentists we focus on the little details and not paid enough attention to the more important factors for long term success. We always look for something or someone else to blame in life when actually we should be looking at ourselves first. If your prep is sub-gingival then you want a cement that is easy to clean up like Ketac Cem. Nowadays there are lots of companies reporting good results with new resin cements for zirconia after sandblasting/priming/silane etc but the long term objective data is yet to be seen. If you see an un-retentive flatter prep it is normally for eMax and not for zirconia (as I try to avoid relying heavily just on bonding for Zr). https://www.nature.com/articles/srep45563
46) I want to work in the UK or be a private dentist like you... Can you help?
Honestly my career in dentistry has not been easy a lot of failures and sacrifices. Instead of buying expensive items I bought my own burs, microscope etc. Nothing I really wanted was given to me. The only advice I have is that anything is possible with the right work ethic and sacrifice. Build a portfolio, find a mentor close to you and do not expect spoon fed answers. Put the work in - you will get much more out! For international dentists wanting to work in the UK, I am not the best person to speak to and have little knowledge on this area please contact the dental council or visit https://www.healthcareers.nhs.uk/explore-roles/dental-team%20/information-overseas-dentists
47) Did you place a post? If so what type and why?
I try to avoid posts as much as possible, but if I do have to place a post I generally prefer a metal custom cast or laser sintered one (anteriorly gold) over a fibre post. I will use parapost for metal or relyx for fibre. I prefer as little prep as possible - just GP removal only. I will even use a prefabricated non engaging metal post depending on the case. The reason I prefer metal post and cores is because I have observed very few failures with these compared to fibre posts but every situation must be judged individually.
48) Did you follow the curve of spee and wilson?
To assess this from a single photograph is not possible (ask any prosthodontist), so do not make judgements without all the information (remember social media is not a replacement for formal education). The curves are important as a guide to recreate an ideal occlusal scheme especially in full mouth rehabilitations. Many times this 'ideal' is for textbooks and not actually conformative to the patients occlusion especially if we are only addressing a quadrant. So if the case is not a full mouth rehabilitation my lab will adjust the shape and angles of the cusps to keep the occlusion comfortable (or the same as original) within the patients own natural envelope of function.
49) Do you always prepare teeth under rubberdam?
In general yes I try to keep supra gingival, if sub gingival I will work under split dam.
50) Why did you crown and why not place a lithium disilicate crown?
Because the bonding and occlusion was not favourable in that particular case. I try to avoid table top preps on heavy para-functional cases. In general I prefer my disilicates to be at least 1.5mm thick occlusally. I often crown a tooth (especially post root canal therapy) to replace an existing failing crown (loss of marginal seal/aesthetics/fracture/periodontal) or provide coverage due to cracks.
51) Why did you polish your preparation?
I generally do a light polish with discs at the end of a prep to refine my margin and profiles. This also makes my impression/scan very smooth and precise which my technician prefers to get an easier adaptation to the margin to the ceramic. A better adaptation means a thinner and more even layer of cement which we all agree helps with overall bond strength. I also tend to cement under rubbderam and after abrasion with 29micron alumina which also aids adhesion. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851321/
52) What is CR?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3732724/
53) What ingot did your technician use?
Normall MT if LiSi. If Zirc normally layered zirconia Argen ht+ shade OM3 with creation Zi-CT. If monolithic normally LAVA Zirc.
54) Did you build your shells one at a time and what about bubbles/dust?
Yes because it gives me more control to build a shell alternatively. Make sure your last increment is one large smooth layer and heated. Do not fold over or add lots of little increments of the composite. Make sure your gloves and instruments are clean of dust and dirt (especially bond/microbrushes).
55) How did you learn to do your work to your level?
Practice Practice Practice and learn from your mistakes. Use magnification for example Bryant Dental dental loupes ideally minimum x4.5/5.0 magnification. I also used and own multiple microscopes such as Zeiss Extaro 300/Labomed/CJ/Zumax/Leica/Global.
56) How can the patient tolerate such long periods of treatment? How do get the patient to accept the treatment plan?
Sedation IV/Oral/Inhalation and/or bite blocks under rubber dam. You always need a great patient, good management and a team that supports you. Regarding treatment acceptance, I discuss all the risks, benefits and costs of each treatment option and simply allow the patient to make an informed choice that best suits them.
57) What is your view on antibiotics in dentistry?
The guidelines state where possible one should avoid prescribing unless medically indicated.
https://bjgp.org/content/66/650/460.3
https://www.evidence.nhs.uk/search?q=antibiotic+prophylaxis+for+dental+treatment
58) What is your view on posts and cores in dentistry? (See no.47 also).
Posts are required to retain the core only they do not reinforce the tooth as commonly believed. The aim should be to retain as much dentine as possible and avoid drilling into the roots where possible. We prefer dual cure cores where possible and air dried canals rather than with paper points and cemented with dual cure cements. We use passive metal dentatus posts, parapost fibre posts and non precious cast and cores where clinically appropriate and patient orientated.
https://onlinelibrary.wiley.com/doi/pdf/10.1111/iej.12847
https://www.researchgate.net/publication/26270297_A_Systematic_Review_of_Dowel_Post_and_Core_Materials_and_Systems
59) What endodontic and implant systems do you use?
For root canals I prefer reciproc and wave one gold with warm vertical condensation or single cone cold lateral where appropriate with AH plus sealant. For implants I tend to use Astra/Ankylos/Straumann/Megagen and prefer guided with custom abutments.
60) Any books you recommend?
Any one of these:
http://www.quintpub.co.uk/index.php?op=productlist&modules=default&act=books&cat_id=111
http://www.quintpub.co.uk/index.php?op=productlist&modules=default&act=books&cat_id=87
http://www.quintpub.co.uk/index.php?modules=default&op=productdetail&act=books&pro_id=591&cat_id=0&nstart=&start=&search_keyword=morphology
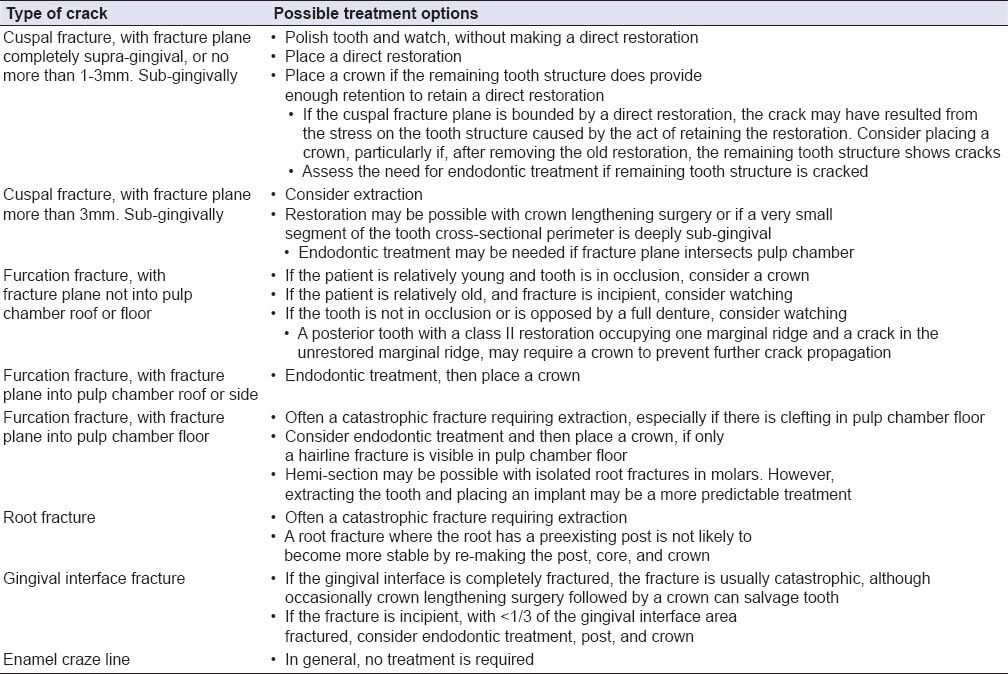
61) What about the crack? How do you manage those?
Have a read of:
https://www.nature.com/articles/sj.bdj.2010.496
https://www.nature.com/articles/sj.bdj.2017.398
https://www.oralhealthgroup.com/features/cracked-tooth-diagnosis-management/
https://www.amjdent.com/Archive/ReviewArticles/2008/Kahler%20AJD%2010-08.pdf
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1834-7819.2009.01155.x
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3633636/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4439863/
The management of cracks will be discussed in more detail on the indirect courses. In many cases you may see very fine crack lines close to the CEJ at preparation margin that I overlay indirectly or with at least 2mm of direct composite material (assuming tooth asymptomatic and the crack is not through and through the tooth). Many times if asymptomatic we will seal the crack (IDS/bioactive bonds and cement) and place a direct or indirect provisional for 2-3 months and observe if symptoms develop or not. It is always important to pre and post warn patients when working on cracked teeth and ensure a photo is taken of the crack to show and explain to the patient what the possible sequelae could be.
This varies depending on case. I have used most brands and in many cases use multiple brands depending on what I want to achieve. Mainly I like to use Supreme, Asteria, GC, Renamel & Hri. I have 2 light cures that I use 3M Elipar DeepCure and VALO by Ultradent (I generally cure min 10 seconds and at multiple angles where possible). Most composites nowadays are very good and that it is mainly operator skill and knowledge provides the best results. I generally try to use a little modelling resin by GC or Brush and Sculpt by Cosmedent. I use GC/Cosmedent no 1 brushes and smile line have angled and non angled auto-claveable versions. If I have used a bulk fill it will be stated under the image (normally we will use filtek one or sdr and build no more than 2-4mm increments) or see below question regarding cores. Composites should retain their polish for at least 3-5 years, the following may help: use a brand with good scientific and long term follow up, layer correctly, use a good curing light, deep glycerine cure, ensure methodical polishing protocol and marginal finishing. For composite and porcelain repairs we tend to use Co-Jet by 3M and on occasion porcelain etch and silane from Ultradent. Remember for anterior bonding success make sure you always check the occlusion and anterior guidance, use strict bonding protocols, provide a night guard or retainer and warn the patient of potential fractures, chips and stains in the future. I try to calibrate my cleaning on a regular basis with caries indicator i.e. Bio clear or Ultra dent or Kuraraye.
2) What liner do you use?
I like Theracal, SDR, ML from GC and superlow flow Tokuyama. The situations I use them and why I discuss on my course. I try not drill away 'healthy' stained tooth tissue where possible and either opaque/abrade or for anteriors internally whiten (google search internal tooth bleaching). We like to use around 1-2mm flowable composite as base liner to the margins, round internal line angles, help with seal and create a radio-opaque masking layer.
3) What brand of rubberdam do you use?
My favourite for photographs is nictone blue heavy (email: [email protected] ps. I do not know any other suppliers), non-latex I like unodent and isodam. I do the majority of my work under rubber dam isolation for patient comfort, improved bonding, control and safety (plus lots more reasons - the benefits of working under dam are endless!). Sometimes if I cannot go through the contact initially I will pre open the contacts with an IPR strip or work under split dam. With onlays (in general we use emax) you may need to use a floss tie to keep the dam seated. With class V restorations I generally work under split dam. I pre wedge for at least 5 mins for all class 2s to allow better seating and haemostasis when I place the dam on. Sometimes the dam looks a different colour during the procedure because of either i) amount of light ii) different brand or shade of dam used iii) sometimes we change the dam during the procedure iv) the flash exposure can be different. We keep the dam clean by doing the following: i) working clean is a mindset ii) wipe the dam clean if needed iii) protect the dam with wedges iv) if there is a tear, loss of seal or amalgam residue I sometimes will change the dam. We prefer to floss secure and place clamp first and then secure the rest (but we change our protocols depending on the situation which we will discuss on the course https://www.youtube.com/watch?v=gfxJUojcmSs). The dam is often changed if we are replacing an amalgam to prevent contamination or if the patient needs a restroom break. Also after air abrasion with ethanol we find the colour of the dam is more matt and is duller (sometimes if handpicks have been over oiled this can create issues).
3) What burs do you use?
I have my own kit available from Komet please contact them on [email protected]. The step by step process of what burs and when is discussed on each teaching module. For occlusal reduction we primarily work on the inclines with a small rugby/flame or round diamond followed by polishing. For preps we like to use the ultrasonic Massironi tip kit also.
4) What camera do you use?
I have a Nikon D7200, D850 with nissin/nikon twin flashes for anterior work with AXIS following eLAB protocol (https://www.emulation.me) and Canon R5 with ring flash +/- polarised filter (polar_eyes) for posteriors when needed. Both with 100 mm macro lens and black out contrasters by smile line (flexipalette). I shoot in both RAW and JPEG backed up on a secure network. My microscope (CJ Optik) runs through a full frame Sony A7Rii and record video at 4K (I prefer camera mounts over mobile). Here is a helpful video about set up and settings: www.youtube.com/watch?v=JQDASOGQp-M
Here are helpful articles about set up and settings:
https://www.nature.com/articles/sj.bdj.2009.607
https://iaaesthetics.com/change-these-6-settings-to-dramatically-improve-your-dental-photography/
With regards to loupes I use x7.5 or microscope for everything including exams. Check out Bryant dental, cj optik and Zeiss. I have a bambach and brumaba ergonomic chairs with arm supports.
5) What matrix do you use?
I like bioclear biofit HD curved (transparent available from bio clear website or optident in UK), tor vm 50micron (silver) and palodent v3 rings. Sometimes for deep margin cases I customise a tofflemire or use a garrison deep margin matrix. I rarely use a Bio-Clear anterior matrix (personal preference) and have my own technique (especially for black triangles) that I discuss on the anterior course. Of recent we have been using polydentia double ring system with a stiff molar matrix. For more information please visit: http://www.polydentia.ch. Other rings and systems such as Garrison etc are fine, if you find what you use works for you then I am happy for you - theres no best system. We tend to build our proximal walls with one shot injection moulding around 1mm thick and cured min 40secs at multiple angles. If we need a large wedge in perio cases we tend to use polydentia haem wedges or the large diamond bioclear wedges. If you see long thin normal wood colour wedges then I am using slim jim wizard wedges by Waterpik.
6) What kit do you use for occlusal carving and layering?
I use the LM arte kit from SI. Namely the fissura and a cosmedent paintbrush (you can also get disposable brush tips from Ivoclar and Smile line). Hu-friedy composite instruments are also recommended. We always like to blend the composite to create smooth margins using the paint brush.
7) What do you use for disinfection? What are the bubbles?
Chlorhexidine solution 2% (www.qedendo.co.uk) and the bubbles are a secret!
8) What cavity preparation or abrasion do you use?
I use twin chamber aquacare by Velopex. I prefer 29micro Alumina and then finish with bioactive glass sylc (1-2 bar) to remove aprismatic enamel rods to ensure no white lines and best possible adhesion.
9) What do you use to cut the gum?
Thermacut bur dentsply or laser. If the margin is a bone level I will carry out sectional surgical crown lengthening to the correct biological width.
10) What clamps do you use?
This varies depending on the situation please attend my course for exact explanations. My own custom rubber dam kit is hopefully coming soon for more information please contact us directly via email.
11) Where have you finished your margin?
I always prefer supra gingival so I can see and create a smooth finish line. I prefer to always finish on sound tooth but sometimes prefer deep margin elevation where I feel more comfortable if it is raised for cementation purposes. I do not recommend that you carry out deep margin elevation in either composite or rmgic without being trained by someone experience as it is one of the most technically demanding procedures in restorative dentistry. If in doubt please refer your case to a periodontist for surgical crown lengthening or a more experienced clinician. Case selection is critical in such cases.
www.sodymd.com.ar/pdf/deep-margin-elevation-a-paradigm%20shit.pdf
www.styleitaliano.org/pdf_article.php?id=11320
With direct composites I always try to remove any unsupported enamel and this drives weather I keep an existing contact or not. If in doubt use an ultrasonic scaler to remove any thin or unsupported tissue whatever is remaining is normally good to retain for bonding purposes post air abrasion. Specific protocols are discussed on the hands on courses.
12) What is injection moulding?
This involves heated composite around 55 degrees (for the benefits of heated composite: https://www.researchgate.net/publication/7770241_Monomer_Conversion_of_Pre-heated_Composite) sometimes with the addition of flowable composite and injected into the cavity and cured multiple times at multiple angles. Here is a video: www.youtube.com/watch?v=6qvaXLNsq0o
13) Do you layer posteriors if so why?
I like layering obliquely as you get multiple cures for a 'strong' restoration and can mimic the beauty of nature. Recreating anatomy requires patience and skill and requires one to develop the fun artistic side of their dentistry. Also by recreating cusp inclines that we see in natural teeth promotes a more stable positive occlusion for patients. In general I will use a dark chromatic dentine shade (a4) followed by a lighter enamel shade (a2/a3). We always try to shade match at the beginning before the dehydration/desiccation effect of the rubberdam (hence sometimes immediately after placement you will see a discrepancy in the colour between the composite and the tooth - within a few hours (if layered correctly) you restoration will be almost invisible. Some people say that replicating anatomy increases the risk of fracture of a composite, to this I can categorically say that in over a decade of layering I have never seen one of my composites split where I have placed a fissure. Although it is true that if your fissures are too deep this can attract food and plaque therefore you must be appropriately trained in such techniques.
14) How do you keep the anatomy?
This is an expansive question which I answer on my course but I advise to always takes a photo of your occlusion before you start and remember your anatomical landmarks. Sometimes you will see a picture where I have restored a fractured or worn cusp with composite and you cannot understand how. This may because I have calculated the room I have available and/or it is part of a full mouth rehabilitation or orthodontic case. Remember do not make judgements when you do not have all the information this is a dangerous. Also I may add that just because some people can do something that you cannot do, does not mean they are wrong and vice versa, always speak to fellow clinicians with respect and assume they are innocent unless proven otherwise. The process of replicating anatomy is discussed on the educational course.
15) What cement and core material do you use?
I generally use heated composite for my core material or a dual cure composite (Ivoclar or G-Aenial GC) but also like to cement with it or variolink esthetic for anterior veneers. The general advice is use a cement and bond made by the same company as they have been designed for optimum bond strength. For RBB's we use PANAVIA 2.0. For posteriors I prefer composite/relyx ultimate or estecem II. A good paper on cementation with composite: www.sciencedirect.com/science/article/pii/S0109564117302579#.WiJMaFfaOAY.facebook
16) Do you treat dentists or HCA's?
Yes I treat many dentists and healthcare professionals, please contact [email protected] or visit www.tahadental.co.uk for referrals. Clinic availability is currently in our custom facility in Oxfordshire only. Also if intra oral photographs and radiographs can be forwarded pre operatively it would help thank you.
17) Could I come watch you at work to observe?
Unfortunately due to the nature of our clientele who want their privacy maintained this is not currently possible. In the future we will be running live patient courses at our training facility please visit www.drth.co.uk/courses.
18) Do you do your anterior work freehand or via a putty stent from a diagnostic wax up?
I always try to do a diagnostic wax up and putty matrix in order to plan the case better. The only time I do not is in an emergency situation where I do a quick A3 body composite mock up without full bonding and create a putty matrix from this. For tooth wear cases we generally get a diagnostically mounted articulated study models in CR (after using the KOIS deprogrammer) and give the patient a night guard at the end of treatment such as a michigan splint if apt.
19) What composite fissure and layering tints do you use?
I like to use the tints kit from Cosmedent (anteriors)/Micerium HFO/Ivoclar brown for posteriors or mix brown and black GC essentia. We normally add tints to reflect nature at the end if it is present in the remaining dentition. Staining/tinting is not essential to function, we recommend that you always discuss this and gain consent from your patient beforehand. Some people say that it does create a more bio mimetic restoration and seals the fissure patterns but this is down to the individual. We layer the tints anteriorly before the final enamel layer and posteriorly as the last addition. I am not worried about wash out as I cure with glycerin gel and find that this is not an issue.
20) Why do you like using zirconia?
Because the soft tissue reacts very well to it (especially if I carry out a vertical or cracked tooth preparation). It is stronger than lithium disilicate. In general I will choose monolithic but in aesthetically demanding cases I will choose layered zirconia . Fit surface is sandblasted 29 micron then Scotch bond/Silane applied and then cemented. One can also use Ivoclean (by Ivoclar Vivadent) to clean the fit surface after try if needed. Most of my bonded posterior indirects will be eMax unless otherwise stated.
21) What is a Vertical or BOPT preparation?
Please visit: www.sweden-martina.com/en_gb/product/bopt_technique-17191/products_for_bopt_technique-17190/bopt_technique-17189.html
22) Do you do any online videos?
Please visit my youtube page (search Dr Thomas Dentist) or visit www.dentinaltubules.com
23) What impression materials do you use?
I currently use 3M impregum soft quick, imprint 4 and honigum by DMG. But also have access to digital scanners such Trios/Medit/iTero.
24) What is your polishing protocol for composites?
We use the Komet, EVE and 3M spiral polishers and finishers with Micerium goats hair brush and sometimes use enamelize paste by Cosmedent (for anterior polishing we normally spend around 15-30 minutes). I also have a specific polishing protocols for different scenarios that I discuss on my course. Heres a quick video: https://www.youtube.com/watch?v=FU7TGWyG-h8
25) What bond do you use?
We generally use Optibond fl and Scotch bond universal. I prefer 4th generation total etch protocols but on occasion (where I deem necessary) I also do carry out selective enamel etch with self etch adhesive (scotch bond or clear fill se). Do not over desiccate dentine.
26) Do you restore one contact at a time?
In general yes as it gives more control. You can start doing multiple contacts in quadrant cases but it depends on cavity design and contact widths needed.
27) Why did you do a composite and not go indirect?
Sometimes the picture you see is part of a longer term plan for the patient and you are just seeing a small window if treatment, which will be restored indirectly at a later date.
if the tooth is heavily restored/cracked or has had a root canal we always generally recommend an indirect cuspal coverage restoration. Some patients due to financial or time restrictions choose composite and are made aware of the risks of their decisions. At the end of the day we as dentists can only guide our patients, give them all the options with the benefits and drawbacks of each, so that they can make an informed decision that is right for them. I would always prefer a direct restoration to doing nothing if a case needs treatment. Sometimes in life we need to pick our battles in order to win the war.
28) What type of temporary do you use?
I tend to use pro-temp or luxa-temp with 3M durelon cement for my temporisation. For veneers we do the same but use spot etch and a little flowable composite if needed.
29) Have you left decayed or stained dentine? Why have you done this?
Sometimes there are a number of factors such as decay, cracks, fractures, overhangs, open margins, lack of contact points, patient symptoms, tooth wear, lack of occlusal function or guidance are just some of the reasons treatment is needed. In regards to decay, generally we tend to clean our cavities with slow speed ceraburs by Komet, air abrasion with 29micron Alumina (Aquacare by Velopex) and then disinfection with Chlorhexidine 2% and then selective enamel acid etch follower by optioned fl. We tend to use caries indicator dye (ultra-dent) and remove all softened decay, if the staining is hard and unaffected we tend to leave this and cover with an opaquer (ML from GC). In some instances if decay is very close to the nerve and on discussion with the patient beforehand we 'may' leave this small area alone as long as the margins are clean (1.5-2.0mm circumferential clearance). We may also then place a bio-restorative material over the top to seal in the area such as bio-dentine or MTA or RMGIC, this will then need to monitored and the patient warned of the increased risk of pulpitis requiring root canal therapy in the future.
You can even do a staged approach if worried:
Caries Management: Step-wise Caries Removal
Stepwise excavation is a method of managing deep/extensive/advanced dentinal caries lesions to reduce the risk of pulpal exposures by removing the caries lesion in separate appointments with ≥ 6 month intervals.
Indications:
- Deep dentinal lesions in teeth likely to result in pulp exposure during excavation
- Evidence of pulp vitality and no evidence of irreversible pulpitis
- No history of spontaneous or continued pain
- Positive pulp vitality (electric, thermal, mechanical)
- Negative to percussion and/or palpation
- Radiographically: >75% through dentine and no periradicular pathology
- Rapidly progressing lesion in a closed cavity
- Stepwise procedure is always discussed with patient before beginning any irreversible treatment
- Stage 1 has the same caries removal goals as selective removal to soft dentin
- Periphery of the cavity should be hard with a clean DEJ resulting in a 1-1.5mm zone of sound and hard dentine
- Perform selective removal to soft dentin, but there should be enough removal of carious tooth tissue to place a durable provisional restoration while still avoiding pulp exposure.
- Undermined enamel can remain at this stage for the retention of a glass ionomer (RMGIC)
- Good sealing with materials that enhance the dentine's ability to remineralize are recommended. Providing a seal is crucial for stoping caries progression. (FDI Policy statement, October 2001)
- Material of choice: Glass Ionomer (Conventional or RMGI). We use glass ionomer Fuji as the initial layer directly over and only over the remaining leathery wet dentin as a visual identifier and then Fuji IX or Fuji II LC is placed on top for functional and cosmetic purposes.
- Check the occlusion
- Re-evaluation and re-entry after ≥6 months
- New radiograph of roots to evaluate for periradicular pathology.
- Check for any symptoms or signs of a possible pulpal inflammation, sensibility and vitality test MUST be carried out.
- Remove the provisional restoration taking care not expose the pulp
- Carry out selective removal of hard dentin centrally (complete removal of initial Fuji layer may not be required to achieve this)
- Place final restoration as indicated with appropriate material to the preparation (think about remaining walls and strength)
- Follow up every 6 months with vitality testing and I would recommend yearly peri-apical radiographs to aid monitoring.
PTFE is fantastic hydrophobic versatile material. We like to roll it up and use it as cord for retraction purposes (it provides great retraction and is gentle to soft tissues). It is also beautifully malleable to pack against matrices to ensure a tight seal is achieved for injection moulding. We also use it to protect teeth during cementation and bonding phases. There are a million other uses for it that I go through on my course - but suffice to say - I love it!
31) Can you tell me more about this procedure?
Occasionally I will post a case that you may have a lot of questions about.... that’s great, but sometimes I cannot go into too much detail for the following reasons:
I) it is not an appropriate case to discuss on social media. The reason for this is that if I explain a procedure on social media someone may replicate it in their own office without formal education and appropriate research - therefore certain procedures are shown just to encourage you to do further research and study. I will sometimes not post certain radiographs and pictures because I do not feel it is appropriate to discuss such cases in a public arena.
II) Some of the stages will not be explained because I have developed my own protocols that I do not want people to copy without having been appropriately taught and explained on my course.
III) To type the answer will take a long time and will most likely start a time consuming conversation that is best left for a formal course.
iv) If I post an X-ray and you think there is decay or an open margin or anything faulty... I can guarantee you that in 99% of the times it is a burn out/artefact or something that I already know about it. Pointing this out to me provides no information and is not helpful and does not make you appear smarter in anyones eyes. Although if you really think I have made a serious error please do private message me as there is always a chance there is actually a genuine mistake... as nobody is perfect all the time.
v) I am not your short cut to knowledge - do not be lazy and do the work yourself. If in doubt start with google. No one ever gave me any short cuts and I am honestly better for it.
vi) If you are really stuck on a case - please contact your nearest more experienced dentist or specialist for advice.
32) How long did this take you and how much do you charge?
In terms of time for a 2 surface direct restoration we normally book around 45mins-1hr (if it is a deep margin or possible crack case we may book up to around 2 hours depending on the complexity and working under microscope). If we are doing quadrants we generally book 3-4 hours. I have found that in dentistry, time is your friend... the more time you have the more relaxed and better your work will be.
With regards to cost, my advice is that dentistry of the highest standard takes more time therefore you should allow for this and your prices should reflect this. If it is a learning or promotional case and this is explained to the patient then a nominal reduction compared to your normal fee is acceptable. Dentistry requires you to take home a salary for your family so if you are giving a lot of discounts you are undervaluing yourself. Work out your hourly rate to make a modest income and charge this - if your patients value you they will not hesitate to pay you for your time and skill.
33) What articulation do you use?
We use Bausch 100u articulating paper (red and blue) and shimstock. We also use an Artex semi adjustable articulator and facebow (also a KOIS dentofacial analyser where apt). In increasing OVD cases (especially in parafunctional patients), we will deprogram for at least 1 week (Kois deprogrammer) and locate CR as our reference. Then a full mouth diagnostic wax up to the prescribed OVD carried out with a facially driven mock up and facebow. We will then go to prototype phase to assess occlusion, aesthetics and phonetics. Once everyone is happy we will go to final ceramics. To learn more about occlusion I suggest you learn from Kois, Spear or Dawson or someone with equal understanding.
34) Is there enough retention in your prep?
If we have 1.5-2mm ferrule and good circumferential enamel (Lakshmi et al 2006 and Singh S et al 2014 then the retention should be very good if a correct bonding protocol is used (discussed on my course). I sometimes can push the limits of bonding with minimal taper and parametric preparations, I do not recommend that you copy these types of preparations as I have been doing them for over a decade and know when and how they should be done and without expert guidance or instruction they can lead to failure. Also when you see an image of a preparation you do not know the full story of occlusion/symptoms/pt factors so please do not create a judgement based on no information this creates fallacies and inaccurate dogmas. What I can achieve under bonding may not be possible for you or vice versa so I advise all clinicians to work within their safe boundaries unless proper mentoring can be provided.
35) Who is your technician and how do you plan?
Due to working with many different technicians it would be unfair to recommend some and not others. I would advise you to discuss complicated cases with your technician before you start a case. Take photos, articulated study models, facebow, bite registration, shade match and check occlusal stops and try to record CR with a kois Deprogrammer or leaf guage for rehabilitation cases.
36) What courses do you recommend?
Mine! lol But seriously just learn from people that do high level dentistry every day in the real world.
37) How do you make your provisionals?
We normally use protemp or luxatemp (using durelon or relyx temporary cement) and for relining we normally follow this protocol attached is a link to a video: https://www.youtube.com/watch?v=cZQNPDmwdfo
38) Can I discuss one of my cases with you?
Due to medico-legal reasons I cannot discuss individual patient cases. However if you provide articulated study models, photos and radiographs on course days, I will be more that happy to discuss possible treatment options.
39) Your contact point looks light/open?
I never post a finished case with an open contact unless otherwise stated. Sometimes due to angulation of the photo or X-ray it may look like this but in reality it is not. Please remember to not make assumptions on someones work without having all the facts. I am an incredibly experienced clinician and have spent my life teaching and posting cases online so it is rare for someone to pose a question to me that I have never heard before.
40) What is the best way to remove silver fillings?
Rubberdam, good ventilation, high speed suction, masks, eye protetection, amalgam sectioning burs (available from Komet) are all essentials. There are some that believe this should be the protocol: https://iaomt.org/resources/safe-removal-amalgam-fillings/
41) Has a dentist ever drilled one of your natural composites by accident? Or do you replace ‘good’ existing fillings?
Not that I am aware of :) and with regards to replacement generally no if there is nothing wrong with the old restoration then I will avoid replacing it unless requested by the patient or to improve cleaning or function.
42) Are your courses CE verified?
Currently we can only provide verification of attendance and hours attended according to UK GDC guidelines (each registration body across the world is different - please check what the requirements are for your own country). In the future we may apply for this or run the course in North America with a registered partner. Whether you can register the course or not... the education you will receive on the course will help your patients from day 1 and improve your level of dentistry, that is what it is all about at the end of the day.
43) Can I do module 2 if I have not done module 1?
Due to current demand delegates that have previously completed module one will be given priority and advance notice. Part of the reason for this is that in module one as you will receive exclusive instructions, equipment and training that will make module 2 easier (especially regarding matrixing and isolation). If you really feel you are ready to go straight for module 2 and skip module 1 then let us know.
44) Can you come to my country to teach?
Yes if it is most likely a lecture but less so if a hands on is required. Currently I only do my 2 day hands on training in London because I organise everything myself (which is a lot of hard work!). The reason I do not let corporates organise anything for my courses (unlike most others) is that they simply do not care enough and there is no attention to detail... I organise everything i.e. the bookings, the venue, the teaching, the microscope, the equipment etc etc so I find it very difficult to trust other people to carry out what I want to the same level as myself. This is mainly because I have been let down by so many people before... sometimes if you want something done right you have to do it yourself. In general I prefer that people attend my course as its the most comprehensive learning I can provide anywhere in the world. Should you wish for me to provide a lecture in the UK & Ireland my fee starts from £3500.00 plus travel and accommodation. For international lectures my fee starts from £5000.00 per day plus travel and accommodation. Remember I put thousands of hours into original slides from scratch to create a custom lecture for each event. So the fee must take that into consideration plus the loss of earnings from travelling. I NEVER lecture for free unless for a charitable cause that I can accommodate. I currently do not do online seminars or lectures as I prefer face to face teaching.
45) Should I use GIC for Zirconia Crowns?
The most important factor with crowns is the preparation and the remaining substrate. Too many times as dentists we focus on the little details and not paid enough attention to the more important factors for long term success. We always look for something or someone else to blame in life when actually we should be looking at ourselves first. If your prep is sub-gingival then you want a cement that is easy to clean up like Ketac Cem. Nowadays there are lots of companies reporting good results with new resin cements for zirconia after sandblasting/priming/silane etc but the long term objective data is yet to be seen. If you see an un-retentive flatter prep it is normally for eMax and not for zirconia (as I try to avoid relying heavily just on bonding for Zr). https://www.nature.com/articles/srep45563
46) I want to work in the UK or be a private dentist like you... Can you help?
Honestly my career in dentistry has not been easy a lot of failures and sacrifices. Instead of buying expensive items I bought my own burs, microscope etc. Nothing I really wanted was given to me. The only advice I have is that anything is possible with the right work ethic and sacrifice. Build a portfolio, find a mentor close to you and do not expect spoon fed answers. Put the work in - you will get much more out! For international dentists wanting to work in the UK, I am not the best person to speak to and have little knowledge on this area please contact the dental council or visit https://www.healthcareers.nhs.uk/explore-roles/dental-team%20/information-overseas-dentists
47) Did you place a post? If so what type and why?
I try to avoid posts as much as possible, but if I do have to place a post I generally prefer a metal custom cast or laser sintered one (anteriorly gold) over a fibre post. I will use parapost for metal or relyx for fibre. I prefer as little prep as possible - just GP removal only. I will even use a prefabricated non engaging metal post depending on the case. The reason I prefer metal post and cores is because I have observed very few failures with these compared to fibre posts but every situation must be judged individually.
48) Did you follow the curve of spee and wilson?
To assess this from a single photograph is not possible (ask any prosthodontist), so do not make judgements without all the information (remember social media is not a replacement for formal education). The curves are important as a guide to recreate an ideal occlusal scheme especially in full mouth rehabilitations. Many times this 'ideal' is for textbooks and not actually conformative to the patients occlusion especially if we are only addressing a quadrant. So if the case is not a full mouth rehabilitation my lab will adjust the shape and angles of the cusps to keep the occlusion comfortable (or the same as original) within the patients own natural envelope of function.
49) Do you always prepare teeth under rubberdam?
In general yes I try to keep supra gingival, if sub gingival I will work under split dam.
50) Why did you crown and why not place a lithium disilicate crown?
Because the bonding and occlusion was not favourable in that particular case. I try to avoid table top preps on heavy para-functional cases. In general I prefer my disilicates to be at least 1.5mm thick occlusally. I often crown a tooth (especially post root canal therapy) to replace an existing failing crown (loss of marginal seal/aesthetics/fracture/periodontal) or provide coverage due to cracks.
51) Why did you polish your preparation?
I generally do a light polish with discs at the end of a prep to refine my margin and profiles. This also makes my impression/scan very smooth and precise which my technician prefers to get an easier adaptation to the margin to the ceramic. A better adaptation means a thinner and more even layer of cement which we all agree helps with overall bond strength. I also tend to cement under rubbderam and after abrasion with 29micron alumina which also aids adhesion. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851321/
52) What is CR?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3732724/
53) What ingot did your technician use?
Normall MT if LiSi. If Zirc normally layered zirconia Argen ht+ shade OM3 with creation Zi-CT. If monolithic normally LAVA Zirc.
54) Did you build your shells one at a time and what about bubbles/dust?
Yes because it gives me more control to build a shell alternatively. Make sure your last increment is one large smooth layer and heated. Do not fold over or add lots of little increments of the composite. Make sure your gloves and instruments are clean of dust and dirt (especially bond/microbrushes).
55) How did you learn to do your work to your level?
Practice Practice Practice and learn from your mistakes. Use magnification for example Bryant Dental dental loupes ideally minimum x4.5/5.0 magnification. I also used and own multiple microscopes such as Zeiss Extaro 300/Labomed/CJ/Zumax/Leica/Global.
56) How can the patient tolerate such long periods of treatment? How do get the patient to accept the treatment plan?
Sedation IV/Oral/Inhalation and/or bite blocks under rubber dam. You always need a great patient, good management and a team that supports you. Regarding treatment acceptance, I discuss all the risks, benefits and costs of each treatment option and simply allow the patient to make an informed choice that best suits them.
57) What is your view on antibiotics in dentistry?
The guidelines state where possible one should avoid prescribing unless medically indicated.
https://bjgp.org/content/66/650/460.3
https://www.evidence.nhs.uk/search?q=antibiotic+prophylaxis+for+dental+treatment
58) What is your view on posts and cores in dentistry? (See no.47 also).
Posts are required to retain the core only they do not reinforce the tooth as commonly believed. The aim should be to retain as much dentine as possible and avoid drilling into the roots where possible. We prefer dual cure cores where possible and air dried canals rather than with paper points and cemented with dual cure cements. We use passive metal dentatus posts, parapost fibre posts and non precious cast and cores where clinically appropriate and patient orientated.
https://onlinelibrary.wiley.com/doi/pdf/10.1111/iej.12847
https://www.researchgate.net/publication/26270297_A_Systematic_Review_of_Dowel_Post_and_Core_Materials_and_Systems
59) What endodontic and implant systems do you use?
For root canals I prefer reciproc and wave one gold with warm vertical condensation or single cone cold lateral where appropriate with AH plus sealant. For implants I tend to use Astra/Ankylos/Straumann/Megagen and prefer guided with custom abutments.
60) Any books you recommend?
Any one of these:
http://www.quintpub.co.uk/index.php?op=productlist&modules=default&act=books&cat_id=111
http://www.quintpub.co.uk/index.php?op=productlist&modules=default&act=books&cat_id=87
http://www.quintpub.co.uk/index.php?modules=default&op=productdetail&act=books&pro_id=591&cat_id=0&nstart=&start=&search_keyword=morphology
61) What about the crack? How do you manage those?
Have a read of:
https://www.nature.com/articles/sj.bdj.2010.496
https://www.nature.com/articles/sj.bdj.2017.398
https://www.oralhealthgroup.com/features/cracked-tooth-diagnosis-management/
https://www.amjdent.com/Archive/ReviewArticles/2008/Kahler%20AJD%2010-08.pdf
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1834-7819.2009.01155.x
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3633636/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4439863/
The management of cracks will be discussed in more detail on the indirect courses. In many cases you may see very fine crack lines close to the CEJ at preparation margin that I overlay indirectly or with at least 2mm of direct composite material (assuming tooth asymptomatic and the crack is not through and through the tooth). Many times if asymptomatic we will seal the crack (IDS/bioactive bonds and cement) and place a direct or indirect provisional for 2-3 months and observe if symptoms develop or not. It is always important to pre and post warn patients when working on cracked teeth and ensure a photo is taken of the crack to show and explain to the patient what the possible sequelae could be.
62) What about veneer try in and cementation?
Most of my ceramic veneers are emax ht or mt or if special aesthetics is needed I will choose feldspathic veneers. Protocols can be found here: https://www.styleitaliano.org/ceramic-veneer-cementation/
https://www.youtube.com/watch?v=y7l2ifaFB0M
For veneer try in I will use water, glycerine, try in paste system of whatever cement system I am using eg. Variolink LC try in paste or one can use something a little stronger for try in such as un-bonded trans flowable.
https://www.dentalsky.com/tetric-evoflow-refill-1x2g-t-ivoclar-vivadent.html
www.ivoclarvivadent.com/en/p/all/products/restorative-materials/composites/tetric-evoflow
Most of my ceramic veneers are emax ht or mt or if special aesthetics is needed I will choose feldspathic veneers. Protocols can be found here: https://www.styleitaliano.org/ceramic-veneer-cementation/
https://www.youtube.com/watch?v=y7l2ifaFB0M
For veneer try in I will use water, glycerine, try in paste system of whatever cement system I am using eg. Variolink LC try in paste or one can use something a little stronger for try in such as un-bonded trans flowable.
https://www.dentalsky.com/tetric-evoflow-refill-1x2g-t-ivoclar-vivadent.html
www.ivoclarvivadent.com/en/p/all/products/restorative-materials/composites/tetric-evoflow
| ips_e-max_clinical_guide.pdf | |
| File Size: | 3189 kb |
| File Type: | |
63) How do I get rid of the white lines in my composites?
Multiple things need to be addressed and be done:
- Get rid of aprismatic enamel with air abrasion 29micron alumina aquacare.
- No unsupported stained enamel, decay left or heavily unsupported tissue.
- Margins modified mini infinity bevel 40 micron diamond and then smoothed with polishers at least 1-2 mm beyond margin (can be slightly wavy if you wish). Sometimes we see this because the reduction and bevel is not enough. People often turn their margins into chamfers which they believe helps. I feel one needs to look at the prep in all directions and ensure no major undercuts or potential areas where white lines could develop.
- Composite (nano or nano hybrid) heated to min 45 degrees. Layered in small increments (no more than 2mm) and blended with paint brush. Try to avoid introducing air bubbles folding the composite over itself.
- Etch beyond margin and do use excess bond over margin (gentle suction).
- Rubberdam isolation is ideal. Try to have a slow 'ramp up' curing light to avoid polymerisation shrinkage stresses. It is suggested small 5 second cures, leave for 4-5 minutes and then a 40 second deep cure.
- Assess whether you need a more opaque composite in thicker proportions slightly beyond the margin.
- Do not polish it all away until the interface is over exposed.
- Final 30-40 second cure under glycerine for oxygen inhibition for better monomer conversion.
Sometimes you have to wait until review or rehydration appointment to see how well you did - do not jump to doing anything drastic initially. If a white line is present which can happen due to the fact the optics of a natural tooth and composite will always be a little different. One can simply reduce the area with a diamond, abrade, follow bonding protocols (co jet/silane) and then re layer. This normally sorts out any issues on review. My advice is really look closely at the area where actually your white line is and make sure you take a photo of your prep and see if you would do anything differently.
64) How do I temporise veneers and do the preps?
https://www.dentistrytoday.com/restorative-134/1859--sp-1757496531
https://www.dentaleconomics.com/science-tech/article/16395078/temporization-for-veneers
https://www.aegisdentalnetwork.com/special-issues/2008/05/provisional-restorations-for-veneer-preparations
https://aacd.com/proxy/files/Dental%20Professionals/jCD/Vol.%2035/Issue%204/34-4_Sisler.pdf
Multiple things need to be addressed and be done:
- Get rid of aprismatic enamel with air abrasion 29micron alumina aquacare.
- No unsupported stained enamel, decay left or heavily unsupported tissue.
- Margins modified mini infinity bevel 40 micron diamond and then smoothed with polishers at least 1-2 mm beyond margin (can be slightly wavy if you wish). Sometimes we see this because the reduction and bevel is not enough. People often turn their margins into chamfers which they believe helps. I feel one needs to look at the prep in all directions and ensure no major undercuts or potential areas where white lines could develop.
- Composite (nano or nano hybrid) heated to min 45 degrees. Layered in small increments (no more than 2mm) and blended with paint brush. Try to avoid introducing air bubbles folding the composite over itself.
- Etch beyond margin and do use excess bond over margin (gentle suction).
- Rubberdam isolation is ideal. Try to have a slow 'ramp up' curing light to avoid polymerisation shrinkage stresses. It is suggested small 5 second cures, leave for 4-5 minutes and then a 40 second deep cure.
- Assess whether you need a more opaque composite in thicker proportions slightly beyond the margin.
- Do not polish it all away until the interface is over exposed.
- Final 30-40 second cure under glycerine for oxygen inhibition for better monomer conversion.
Sometimes you have to wait until review or rehydration appointment to see how well you did - do not jump to doing anything drastic initially. If a white line is present which can happen due to the fact the optics of a natural tooth and composite will always be a little different. One can simply reduce the area with a diamond, abrade, follow bonding protocols (co jet/silane) and then re layer. This normally sorts out any issues on review. My advice is really look closely at the area where actually your white line is and make sure you take a photo of your prep and see if you would do anything differently.
64) How do I temporise veneers and do the preps?
https://www.dentistrytoday.com/restorative-134/1859--sp-1757496531
https://www.dentaleconomics.com/science-tech/article/16395078/temporization-for-veneers
https://www.aegisdentalnetwork.com/special-issues/2008/05/provisional-restorations-for-veneer-preparations
https://aacd.com/proxy/files/Dental%20Professionals/jCD/Vol.%2035/Issue%204/34-4_Sisler.pdf